Estudio de investigación Ejercicio correctivo
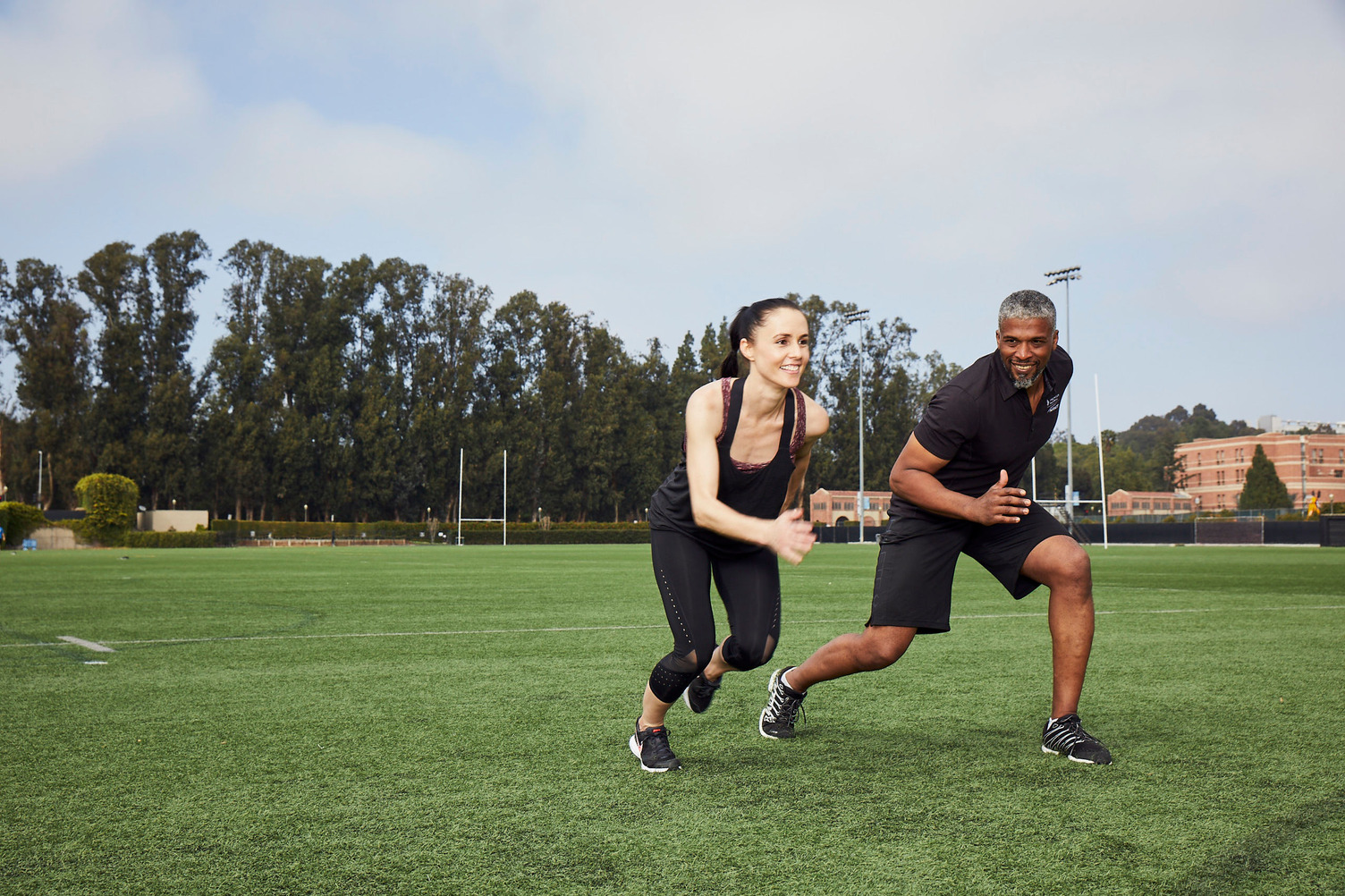
Research Review Effects of Selected Rehabilitative Exercises on External Rotator Muscles and Trapezius Muscles of Masonry Workers Study Author Singh, G. K., Srivastava, S., Kumar, M., & Ratnakar, S. Original Citation Singh, G. K., Srivastava, S., Kumar, ...
¿Con qué frecuencia escuchas preguntas como: "¿Cuánta proteína debo consumir?" "¿Qué opinas sobre el ayuno intermitente?" "¿Debo seguir [insertar el nombre de la dieta popular actual] para perder peso?" No es sorprendente. La nutrición y el estado físico ciertamente no pueden ...
Entrenador personal certificado destacar Fitness juvenil
Podemos tambalearnos en el uso del término "encajar" para referirnos a la salud y el bienestar de una familia, pero eso con demasiada frecuencia puede abarcar la noción de que las metas de una familia son performativas. Estar BIEN es la meta.
Nutrición destacar hipertrofia
Ganar músculo no es tan fácil como ir al gimnasio y levantar pesas. Esa es solo una parte de la ecuación. En realidad, ganar músculo requiere dos cosas principales: un estímulo para el crecimiento y la energía para desarrollar tejido.
Entrenador personal certificado estrés destacar
El estrés estimula el apetito, aumenta la grasa abdominal, aumenta los riesgos de enfermedades e incluso puede influir en nuestras relaciones íntimas. La lista podría continuar, pero ¿qué es exactamente el estrés y cómo se relaciona con todas estas consecuencias?
Revista Estadounidense de Fitness trx Revista American Fitness Otoño 2020 destacar
Publicado originalmente en la edición de otoño de 2020 de American Fitness Magazine. Cuando Randy Hetrick "MacGyvered", el predecesor del TRX® Suspension Trainer ™ actual, mientras se desempeñaba como oficial de los Navy SEAL en 1997, no tenía idea de que estaba creando un nuevo ...
El cuidado personal es una palabra que sigue apareciendo en artículos de noticias y correos electrónicos de empleados de toda la empresa durante la pandemia de coronavirus. Debido al estrés sin precedentes que enfrentan muchas personas, algunas empresas están restableciendo su Programa de Asistencia al Empleado (EAP) ...
Sportstraining-Weightloss y AFAA son los administradores de lo que significa ser el mejor y el más brillante en fitness y bienestar. Ambas marcas están enfocadas en construir una comunidad diversa y única dedicada a crear un futuro mejor y más brillante en la industria.
Entrenador personal certificado destacar
El ejercicio a menudo se asocia con esfuerzo físico y adaptaciones como pérdida de peso, mejor rendimiento atlético y aumento de la fuerza. Sin embargo, una cosa que todas estas variables tienen en común es que no son inconscientes.
Entrenador personal certificado CPT Q & A destacar
Si eres fanático de la televisión diurna, probablemente reconozcas a Sal Stowers. Es una habitual de Days of Our Lives de NBC, donde interpreta a la detective de policía Lani Price. Sin embargo, como verá, eso es solo una pequeña parte de quién es ella y de lo que le apasiona ...
















.jpg?width=357&name=Optima%20Ads_blog3%20(1).jpg)